Cervical Screening
Cervical screening

Regular cervical screening is your best protection against cervical cancer (external site). Most people who develop cervical cancer in Australia have either never screened or do not screen regularly.
In Australia, all women and people with a cervix aged 25 to 74 years who have ever had any sexual contact should have a Cervical Screening Test every 5 years.
There are now two ways to have a Cervical Screening Test
You can choose to:
- take your own sample, or
- have your healthcare provider collect your sample
Self-collected |
|---|
|
A self-collected Cervical Screening Test |
|
✅ You collect your own sample from the vagina |
|
✅ Checks for HPV |
|
⚠ Does not collect cervical cells to check for abnormal cell changes |
|
⚠ If HPV is found, you will need to return to have a cervical sample collected by your healthcare provider or specialist to check for abnormal cell changes. |
 |
Clinician-collected |
|---|
|
A healthcare provider-collected Cervical Screening Test |
|
✅ Your healthcare provider collects a sample from your cervix containing cervical cells. |
|
✅ Checks for HPV |
|
✅ If HPV is found, the same sample is checked for abnormal cervical cell changes. |
|
|
 |
Being screened regularly means that the human papillomavirus (HPV) and any changes it may cause to the cells of the cervix can be found early. These cell changes can then be monitored and, if needed, treated to prevent cervical cancer.
What is human papillomavirus (HPV)?
There are many types of HPV infections and most are cleared naturally by the body’s immune system within one to two years without causing problems.
HPV is a very common infection that is spread through any sexual contact. HPV is so common that many people have it at some point in their lives without knowing as there are usually no symptoms.
In some cases, a HPV infection that is not cleared by the body can cause abnormal cervical cell changes. If left undetected and/or untreated, these changes can develop into cervical cancer. It usually takes more than 10 to 15 years for a persistent HPV infection to develop into cervical cancer.
Access the HealthyWA website (external site) for more information on HPV.
The HPV vaccine (external site) can protect against some types of cancer-causing HPV, including types 16 and 18. Since the HPV vaccine does not protect against all types of HPV known to cause cervical cancer, HPV vaccinated women and people with a cervix still need to have regular cervical screening.
Do I need cervical screening?
All women and people with a cervix aged 25 to 74 years who have ever had any sexual contact should have regular cervical screening.
This includes those who:
- feel well and have no symptoms
- are pregnant
- have been vaccinated against HPV
- are going through menopause
- no longer have periods
- have not had sexual contact for a long time
- have only ever had one sexual partner
- have an intellectual or physical disability
- only have sex with women
- are transgender, gender diverse or non-binary and have a cervix.
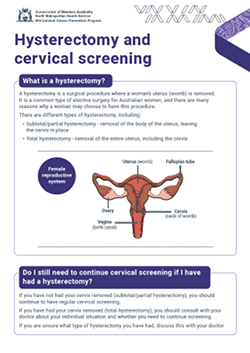
If you have had a hysterectomy, speak with your healthcare provider to check if you still need to screen.
Cervical screening is for women and people with a cervix who are well without any unusual signs or symptoms. See your healthcare provider if you have any of these symptoms:
- vaginal bleeding after sex
- bleeding between periods
- vaginal bleeding after menopause
- unusual vaginal discharge
- continual pain during sex.
If you are unsure of when you are due to screen, please speak with your healthcare provider or contact the National Cancer Screening Register on 1800 627 701.
When am I due to screen?
The National Cancer Screening Register (NCSR) (external site) sends participants invitations and reminders to screen via the post or SMS. If you are unsure of when you are due to screen, please speak with your healthcare provider or contact the NCSR on 1800 627 701.
Where can I have a Cervical Screening Test?
You can have a Cervical Screening Test at your:
- GP practice
- Sexual Health Clinic
- Aboriginal Medical Service
- Women’s Health Centre
- Community Health Clinic.
Your Cervical Screening Test may be taken by a GP, nurse, midwife or Aboriginal health practitioner, or you can choose to collect your own sample.
Ask about any costs when you make your appointment. It is important to find a healthcare provider you trust, at a service where you feel comfortable. You can request a healthcare provider of the gender you prefer when you make your appointment. Make sure you tell the receptionist the appointment is for a Cervical Screening Test as you may need to book a longer appointment.
Find out more about where you can have a Cervical Screening Test (external site).
Understanding my test results
Your healthcare provider will discuss the results of your Cervical Screening Test (external site) with you.
Access the HealthyWA website (external site) for more information on understanding your Cervical Screening Test results.
Cervical screening for health professionals
Education and resources for health professionals can be found on the education and resources for health professionals – cervical screening page.
WA Cervical Cancer Prevention Program
The WA Cervical Cancer Prevention Program (WACCPP) is the state arm of the National Cervical Screening Program (NCSP). For more information about the WACCPP visit Cervical Screening – WA Cervical Cancer Prevention Program.